The development of a pressure ulcer (PU) is a multifaceted process, a cascade of events triggered by sustained pressure and influenced by a complex interplay of intrinsic and extrinsic factors. While pressure itself is the primary initiating factor, acting as the inciting event, other elements – such as shear forces, friction, moisture levels and the patient’s overall health and physiological status – play critical, and often synergistic, roles.
According to the National Institute for Health and Care Excellence (NICE), over 700,000 people are affected by PUs in the UK alone each year. A thorough understanding of these contributing factors and their intricate interactions is fundamental to implementing effective, targeted prevention strategies of PUs in Intensive Care Units (ICU). ICUs, by their very nature, present a unique and formidable challenge in the prevention of pressure ulcers. ICU patients are, by definition, critically ill. These individuals are often suffering from multiple, complex comorbidities and are frequently undergoing aggressive, life-sustaining medical interventions. This is significantly compounded by several factors that directly and dramatically increase the risk of tissue breakdown and PU formation.
Burdening ICUs
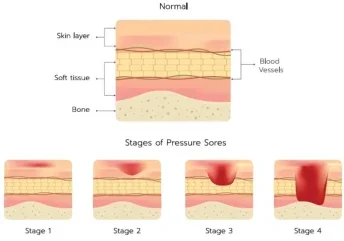
Patients who are deeply sedated, requiring mechanical ventilation or suffering from neurological impairments, such as stroke or spinal cord injury, are simply unable to reposition themselves voluntarily and regularly. This prolonged, unrelieved pressure restricts blood flow to the overlying skin and underlying tissues. This restriction leads to tissue ischemia, a state of oxygen deprivation that results in tissue necrosis – the death of cells and tissues.
The duration of this unrelieved pressure is a critical determinant of the extent and severity of tissue damage. Even relatively short periods of sustained pressure, particularly in individuals with compromised circulation, can lead to irreversible tissue harm. Repositioning schedules are a standard practice in ICUs; however, their effectiveness relies heavily on strict adherence by nursing staff and, even with meticulous implementation, may prove insufficient for patients at extremely high risk of PU development. The physiological instability, which is a hallmark of critically ill patients in the ICU, further exacerbates the risk of pressure-induced tissue damage. Conditions such as sepsis, septic shock and cardiogenic shock, all of which compromise cardiovascular function, significantly impair tissue perfusion. This reduced blood flow makes the skin and underlying tissues markedly more susceptible to pressure-related injury.
Vasopressor medications, frequently used to maintain adequate blood pressure in critically ill patients, can further reduce peripheral blood flow, potentially contributing to tissue hypoxia and increasing the risk of ulceration. Continuous monitoring of vital signs, including blood pressure, heart rate, oxygen saturation and indicators of tissue perfusion, such as capillary refill time and skin temperature, is crucial for identifying patients at increased risk and tailoring preventative interventions accordingly. Beyond circulatory compromise, respiratory dysfunction – another common problem for ICU patients – can contribute significantly to PU development. Hypoxia, a state of inadequate oxygen delivery to the tissues, directly impairs cellular metabolism and viability, hindering the skin’s ability to withstand pressure and delaying wound healing should an ulcer develop.
Mechanical ventilation, while a life-saving intervention for patients with respiratory failure, can increase the risk of PUs due to prolonged immobility and the potential for pressure from the ventilator tubing, mask interfaces and endotracheal tube securing devices. Careful attention to securing these devices, using appropriate padding and pressure-relieving materials, and regularly assessing the skin beneath them is essential to minimise this risk.
Malnutrition, often present and frequently overlooked in critically ill patients, significantly weakens the skin’s resilience and its inherent ability to resist pressurerelated damage. Protein-calorie malnutrition, in particular, impairs collagen synthesis, a crucial process for maintaining the skin’s tensile strength and structural integrity. This reduction in collagen makes the skin more fragile and susceptible to breakdown. Deficiencies in essential micronutrients, such as vitamin C, zinc and copper, all of which play vital roles in wound healing and tissue repair, further compromise tissue integrity and increase the risk of ulceration.
A comprehensive nutritional assessment and adequate nutritional support are, therefore, integral components of any effective PU prevention strategy. This often requires a multidisciplinary approach, involving registered dietitians, nurses and physicians, working collaboratively to optimise the patient’s nutritional intake, whether through oral feeding, tube feeding or intravenous feeding.
Multifaceted preventative strategies
Effective PU prevention in the complex and demanding environment of the ICU extends far beyond the traditional practice of simply repositioning the patient at regular intervals. While regular turning remains a fundamental and essential element of any prevention protocol, a comprehensive, multifaceted approach, incorporating pressure redistribution, meticulous skin care, optimal nutritional support and continuous, vigilant monitoring, is required to minimise the risk of these devastating complications.
Pressure-redistributing support surfaces are a cornerstone of modern PU prevention strategies. Standard hospital mattresses, typically designed for comfort and general support, are generally inadequate for providing sufficient pressure relief for high-risk, immobile patients. Dynamic support surfaces, such as alternating pressure mattresses and overlays, actively and dynamically redistribute pressure by cyclically inflating and deflating a series of air cells within the mattress or overlay. These mattresses and overlays are used by a number of NHS trusts throughout the UK.
These devices have been consistently shown in numerous clinical studies to be significantly more effective than static surfaces, such as standard foam mattresses, in reducing the incidence of PUs, particularly in high-risk populations. In a 2020 study by the National Institute for Health and Care Research, it was found that Grade 2 PUs took on average 18 days to develop on an alternating pressure mattress as compared to 12 days on regular hospital mattresses – an improvement of 50%. Additionally, low-air-loss mattresses provide a constant flow of air through small perforations in the mattress surface, helping to keep the skin dry and cool, which is particularly beneficial for patients with moisture-related skin problems. Heel protection devices, such as specialised boots, pillows, foam wedges or heel protectors, are essential for preventing heel ulcers, a common and often very difficult-to-treat complication, particularly in patients with compromised circulation or peripheral neuropathy.
Regular skin assessments, ideally performed at least once per nursing shift and more frequently for patients identified as being at very high risk, are vital for the early detection of any signs of pressure damage.
These assessments should include a thorough and systematic inspection of all bony prominences, areas of skin folds, and any areas exposed to moisture, friction or shear forces. The use of standardised skin assessment tools and documentation protocols can improve consistency and accuracy. Meticulous skin care is an essential element in maintaining skin integrity and preventing breakdown. Gentle cleansing with pH-balanced cleansers, avoiding harsh soaps or excessive scrubbing, which can damage the skin’s protective barrier, is critically important. The application of barrier creams, ointments or films protects the skin from the damaging effects of moisture and irritants, such as urine, faeces and wound exudate.
These products create a protective layer that reduces friction and prevents maceration, the softening and weakening of the skin due to prolonged exposure to moisture. Managing incontinence effectively, with prompt cleansing and the use of absorbent pads, briefs or specialised containment devices is crucial. Careful attention should also be paid to managing perspiration and wound exudate, ensuring that the skin remains clean, dry and intact.
Technologically optimising care
The field of pressure ulcer prevention is undergoing a period of rapid evolution, with technological advancements offering new and increasingly sophisticated tools and strategies to enhance patient care and improve outcomes. Continuous bedside pressure mapping (CBPM) systems provide real-time feedback on pressure distribution at the patient-support surface interface. These systems utilise an array of sensors, typically embedded within a mattress overlay or pad, to create a dynamic, visual map of pressure points, allowing clinicians to identify areas of sustained high pressure and adjust patient positioning accordingly. According to a 2014 study in the American Journal of Critical Care, CBPM can significantly reduce the incidence of PUs to 0.9% of patients compared with 4.9% in the control group.
The development of “smart” textiles and “intelligent” dressings represents another promising area of innovation. These advanced materials can detect subtle changes in pressure, moisture, temperature and even biochemical markers of early tissue damage, providing early warning signs of potential skin breakdown and allowing for timely intervention. Some of these dressings are also designed to actively promote wound healing by releasing therapeutic agents, such as growth factors, antimicrobial agents or anti-inflammatory medications, directly to the wound site, accelerating the healing process and reducing the risk of complications. AI and machine learning algorithms are increasingly being applied to the challenge of PU prevention. These sophisticated algorithms can analyse vast amounts of patient data, including demographic information, risk factors, vital signs, laboratory results, medication profiles and pressure mapping data to predict the likelihood of PU development with a high degree of accuracy. This allows for more targeted and proactive preventative interventions, focusing resources and attention on those patients identified as being at greatest risk. AI-powered systems can also help to optimise repositioning schedules, identifying patterns of pressure loading that might be missed by human observation, and even suggesting personalised care plans, tailoring interventions to the individual patient’s specific needs and responses to treatment.
Beyond the implementation of advanced technologies, effective communication and seamless collaboration within the healthcare team are essential for successful PU prevention. Regular team meetings, clear and concise communication protocols, and shared decision-making processes ensure that all aspects of the patient’s care are carefully coordinated and aligned, maximising the effectiveness of prevention efforts. Comprehensive education and ongoing training are also vital components of any successful PU prevention programme. Continuing professional development for all staff members involved in direct patient care, covering topics such as risk assessment methodologies, skin assessment techniques, proper positioning and offloading techniques, the use of pressure-redistributing devices and nutritional management is essential for maintaining a high standard of care and promoting a culture of prevention within the ICU.
The fight against PUs in the critically ill patient population is a continuous, multifaceted and demanding undertaking, requiring unwavering vigilance, continuous innovation and a steadfast commitment to patient wellbeing. By embracing a holistic, proactive and evidencebased approach, incorporating the latest technological advancements and fostering a culture of collaboration and continuous improvement, the incidence and devastating consequences of these largely preventable complications can be significantly minimised.





