Ventilator-associated pneumonia (VAP) is a common menace within intensive care wards. Affecting around 20% of critically ill patients, this is a serious lung infection that can occur after a person has been on a ventilator for 48 hours. Estimating its mortality rate can be tricky – this is a patient pool who, after all, are already sick enough to be intubated. However, we know that it increases the average length of hospital stay by around four to nine days, and that it bumps up treatment costs by around £9,000 per patient. It also accounts for around half of all antibiotic use within the ICU, as doctors aim to halt the spread of bacteria. While VAP is far from a new problem, awareness grew significantly during the peak of the Covid-19 pandemic. Many mechanically ventilated patients, who were in the ICU for severe Covid-19, subsequently contracted VAP as well. Not surprisingly, this was associated with even worse outcomes. In one study of 1,424 ventilated patients, 231 had VAP episodes. Among those without VAP, 44.7% died within 60 days, compared to 47.6% of those who had contracted an additional infection.
“This underlines the point that people who are put on mechanical ventilation tend to be very sick to start with,” remarks Dr Freya Harrison, a microbiologist working in the School of Life Sciences at the University of Warwick. “You’ll have a subset of people who were young, healthy adults, who had an accident and ended up being ventilated, but most people will have an underlying immune issue or infection. So they might have Covid-19, they might have COPD, they might have conditions like diabetes that reduce their ability to fight infection.”
The upshot is that VAP can be hard to eradicate. Although antibiotic treatment does sometimes clear the infection, VAP recurrences are common, and the bacterial biofilms often persist on the ventilator tubes. Factor in any underlying health conditions or immune disturbances, and it’s easy to see why patients remain so vulnerable.
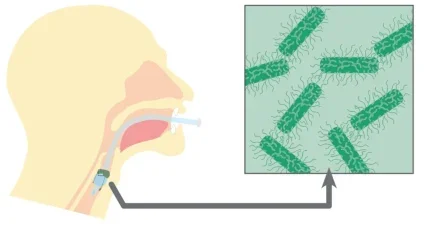
“With any indwelling medical device, you’re providing a surface for infection,” says Harrison. “Add in the fact that, if you’re on a ventilator, you’ll be sedated, you’ll be lying down, so your cough reflex is gone. You can’t clear your secretions. So you have this horrible situation where all of your oropharyngeal secretions will pool around this tube in your throat.”

Possible solutions have been suggested. For instance, patients will be laid prone on their front – a more desirable angle for clearing secretions – or the healthcare team may try to physically clear those secretions using a suction tube. There are also tubes on the market with antimicrobial coatings, which have performed fairly well in clinical trials. However, none of these options represent a silver bullet. The suction tube can come with added risk to the patient, while the coated tubes are not very cost-effective considering the scope of their benefits. “It’s really interesting to compare this with something like wound care, where you have all of these advanced dressings with additions that try to prevent bacterial or fungal colonisation,” notes Harrison. “We’re not there yet with these tubes – they don’t have a great impact on reducing colonisation.”
Fighting for air
The research community is intent on finding better answers. One possible option, pioneered by Viromed Medical in Germany, is cold plasma therapy, which has already proved successful in treating hard-to-heal wounds. Cold plasma holds great promise compared to traditional antimicrobial treatments: it can reach the site of infection within a few minutes, where it destroys pathogens physically, even those that have grown resistant to antibiotics.
“If the positive preliminary results of our study are confirmed, cold plasma could revolutionise the treatment of ventilated patients,” said Professor Hortense Sleveogt of the Hanover Medical School, who is leading the project’s scientific direction.
Another possible strategy might be to administer probiotics. If given to all mechanically ventilated patients, they might help reduce the incidence of VAP, while slashing antibiotic usage. Amid some rather mixed results, some studies have suggested there might be a significant benefit. Researchers are also working on monoclonal antibodies and vaccines for VAP. While this work remains at an early stage of development, these kinds of treatments could be a gamechanger within a post-antibiotic era. Other teams, meanwhile, are exploring rapid sensitivity testing, which will improve diagnosis and enable patients to be treated with better targeted antibiotics.
Harrison’s team at the University of Warwick are less interested in finding new treatment strategies, and more in improving the basic state of research in the field. In August 2024, they published a paper in the journal Microbiology, detailing a recent breakthrough. By creating an accurate model of hospital conditions, they were able to learn more about the behaviour of the underlying pathogens. They were also able to run experiments, discovering which treatment strategies might work best.
“Companies could use this model to help find new drugs and new tube coatings to prevent VAP,” comments Harrison. “I like the idea of making something that allows us to study microbiology in a new way but might also produce something useful.”
Stubborn infections
Unlike typical lab models, which are not particularly accurate, the researchers’ new model provides a good simulation of what happens within the ventilated patient’s airways. They used the same type of tubes that are deployed in real-world settings, along with a ‘synthetic ventilated airway mucus’. This is a strategy that has been deployed for cystic fibrosis previously, but never for VAP.

“We were aware of studies where people had taken real endotracheal tubes, and put them in a microbiological growth medium,” says Harrison. “But that was a standard lab medium that doesn’t actually mimic the chemistry inside an infected host. We were able to review the literature, come up with a current best guess of how we could make synthetic ventilated airway mucus, and then combine that with sections of tube to see how bacteria and fungi grew on them.”
VAP, she notes, is fundamentally a biofilm infection. Invading bacteria – which may come from the patient’s own body or from the healthcare environment – form tight-knit communities on the surface of the tube, encased in a slimy matrix. The researchers wanted to see if they could grow biofilms on the tubes, akin to the ones that occur in patients. They found that they could. What’s more, the biofilms in question were strikingly hard to eradicate. In contrast to typical lab models, in which antimicrobial treatments are quite effective, these bacterial and fungal species were stubbornly averse to treatment. High concentrations of antimicrobials were required to have any effect – comparable to what you’d find in a real-world setting. The biofilms were also extremely thick, consistent with previous studies that have examined the tubes extubated from patients. Up to 84% of these tubes are completely covered in biofilm, increasing the likelihood of VAP. On a more encouraging note, the researchers found that combining antibiotics with ‘matrix degrading enzymes’ represented a promising treatment strategy. These enzymes, which break down the biofilm’s protective slime layer, made the bacteria more vulnerable to attack and allowed the researchers to halve the concentration of antibiotics needed.
“The problem with VAP is that if you start to break down a biofilm, it’s got nowhere to go except the lungs,” points out Harrison. “We’d have to be very, very careful that we weren’t just moving the bacteria. So how useful it would be, I don’t know. But it is a proof of principle that if you can combine something that breaks down that biofilm matrix with an antimicrobial, you can improve treatment.”
Searching for answers
Harrison sees her work more as a starting point for fellow researchers, who might be interested in finding new drug targets and working out what kind of drugs are most appropriate. Ultimately, she would like to develop two versions of the model – an open-access version for those conducting fundamental research, and another for commercial purposes. Recently, her team received a grant from the National Biofilms Innovation Centre to work with a local robotics and 3D printing specialist. Together, they are looking to design a 3D printed bivalve ventilator, with a view to improving their model of the patient’s body. The attraction of these kinds of models, she says, is not just that they’re more naturalistic; they could also help eradicate animal research.
“The animal model of VAP is really horrible – if you’re having to ventilate a mouse or a pig, it’s a really invasive procedure,” says Harrison. “It’s one of those areas where, if we can replace animal use, it’ll have a massive ethical impact, as well as potentially being more informative.”
Although VAP is a stubborn problem, which continues to fox healthcare systems across the world, Harrison is confident that there will be ways to improve on the standard of care. “My personal gut feeling is you’re going to have to have a combination of a new kind of tube with an antimicrobial treatment,” she says. “I don’t think we’re going to find a magic tube that prevents any host tissue or bacteria from sticking to it, but we might be able to find something that’s a bit better than what we’ve got.”





