Symptoms and complications of acute gastroenteritis have led to a considerable disease burden due to growing health system use and productivity loss. For example, in the Netherlands and Belgium, annual direct medical costs of acute gastroenteritis amount to €945m and €112m respectively. Similarly, in Finland, productivity loss and the associated cost of lost workdays has been estimated at €1.8–2.1m with the prevalence of participants on sick leave recorded at 3.54 times higher in the week following an outbreak.
Fast testing is vital
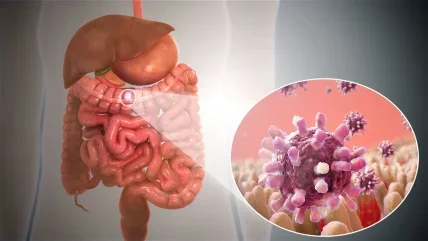
As infants and the elderly are particularly susceptible to complications arising from acute gastroenteritis, rapid provision of test results helps guide medical professionals to the appropriate treatment type for critical care patients. Furthermore, given the highly infectious nature of the disease, hospitals find themselves short of isolation facilities. Beds are limited and are in high demand for non-infectious patients, let alone for patients requiring isolation to prevent the spread of gastroenteritis.
Fast testing for gastrointestinal infections may reduce the time spent in isolation for some patients, therefore reducing overall associated burden.
The introduction of Nucleic Acid Amplification Tests (NAATs) bridged the gap between conventional methods of diagnosis and the higher performing molecular diagnostic (MDx) techniques. NAATs have been consistently shown to be more sensitive and specific compared to non-nucleic acid-based methods. For viral acute gastroenteritis, diagnosis can be made more quickly in the course of the infection even when there are low levels of viral shedding. NAATs identify the pathogen in question irrespective of culture constraints and demonstrate good reproducibility between laboratories.
MDx testing in symptomatic individuals has become increasingly sophisticated over the past 20 years and these diagnostic tools for infectious acute gastroenteritis have undergone several innovations from scatological cultivation to next-generation sequencing (NGS).
Commercially available MDx-based assays have changed the way laboratory diagnosis of enteric infections are performed. Although reagent and instrument costs are higher for real-time PCR technology compared to conventional techniques, the level of automation that comes with this technology significantly reduces hands-on time per specimen to as little as two minutes. The automated efficiency makes this kind of targeted MDx far less labour intensive compared to traditional techniques.
PCR pragmatism
PCR tests have been shown to consistently result in high diagnostic values with >90% sensitivity and close to 100% specificity. Multiplex PCR-based testing simultaneously evaluates stool specimens for the presence of multiple pathogens, whereas single PCR-based platforms target specific pathogens. Highly multiplex panels do run the risk of providing false-positive results in the case of rare pathogens. In addition, it is important that the platform is integrated and does not require separate nucleic acid extraction and post-PCR handling in order to prevent contamination and false positives. When these criteria are met, a targeted syndromic approach can be used to test several pathogens known to cause the same syndrome in patients. Integrated multiplex platforms have a substantial impact on patient management in comparison to single PCR-based platforms, with the potential to reduce the time to first identification of a pathogen, influence patient outcome through early initiation of targeted antibiotic therapy, alter antimicrobial stewardship and finally, optimise infection control.





