In 2023, a patient with an urgent need for knee replacement surgery presented at the Heidenheim Klinikum. However, a complex medical history, advanced age and a number of complicating factors meant that a straightforward approval for surgery was not possible.
At 70 years of age, the patient was admitted for a consultation having suffered years of knee pain. Analgesics and physiotherapy had proven unsuccessful in treating her condition. In many cases, the consultation for prosthetic knee surgery would have been relatively straightforward, but her comorbidities made the decision less clear cut. The patient had a secondary diagnosis of diabetes mellitus, though it was well managed with an HbA1c below 7%. Furthermore, she was clinically obese at the time of admission with a body mass index (BMI) of 45 kg/m2.
“The patient has severe osteoarthritis of the knee – a Kellgren and Lawrence Grade 4, which can mean a marked narrowing of the joint space, severe sclerosis and deformity of the bone ends,” says Helwig. “She had a limited range of motion with extension deficit, and her pain on the visual analogue scale (VAS) was a nine. And, according to the guidelines in Germany, we are not supposed to operate on patients with a BMI above 40.
“If range of motion is so bad and osteoarthritis is so extended, then there is the possibility of losing more bone through the condition and making the operation later more complicated,” he adds. “The patient was suggested bariatric surgery to help with weight loss, even though bariatric surgery is up to recent years rarely done on patients at the age of over 65 years. But even if she had lost weight, she would have to wait one or two years. With this in mind, I decided to do the knee surgery as one of two suboptimal possible decisions.”
The highest standards of hygiene
The level of obesity made the procedure far more challenging than most cases. The surgery to fit the knee prosthesis was atypical in many respects. For example, the time between incision and suture (incision to closure time) was longer than normal.
“The procedure is not too challenging normally but, in this instance, it took more time,” remarks Helwig. “Usually, it takes around 60 minutes to perform a total knee prosthesis with the system we used, but this time it took 115 minutes because of exposure of the joint and the condition of the patient. This is not extraordinarily long but longer than our average patient and almost longer than suggested from the German orthopaedic society.”

Hygiene and safety are always paramount in the operating theatre, but with a longer exposure to the external environment in this procedure, there was even more emphasis than usual on keeping the implant the surrounding tissues clean and free from infection. A key part of the solution could be the use of PREVENTIA Surgical Irrigation, a new antimicrobial surgical wound irrigation fluid from German company Paul Hartmann AG, which has been innovating in the medical technology sphere for more than 200 years, but was not available at the time of surgery.
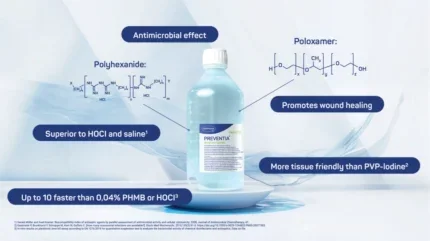
PREVENTIA Surgical Irrigation consists of a unique combination of two active substances. The first is polyhexanide (PHMB), which has a broad spectrum of antimicrobial qualities and is highly effective against biofilms. PHMB kills bacteria which are part of biofilms and provides a robust defence against harmful microbes. Therefore, it penetrates the cell membranes of bacteria, where it causes an instability of the membrane structure, inside the bacterial cell it binds to the DNA. The second substance is poloxamer, a synthetic copolymer consisting of hydrophilic polyethylene oxide (PEO) and hydrophobic polypropylene oxide (PPO). This works as a surfactant that reduces the tension between two materials. This allows the active ingredient PHMB to reach its site of action more effectively and supports the removal of affected tissue during debridement.
“The main advantage of using this product is in the prophylaxis to rinse the operation site at the end of the surgery. In addition, it can be used in already infected cases,” Helwig explains. “It provides the effect of mechanical irrigation and an antimicrobial effect. Using PREVENTIA Surgical Irrigation means we have a better effect against potential infections. The two substances in PREVENTIA Surgical Irrigation – an agent against microbes and a surfactant – together prevent the formation of biofilms, and also deliver a strong antimicrobial effect.
“Using PREVENTIA Surgical Irrigation means we have a better effect against potential infections.”
The substance is more tissue-friendly than povidone-Iodine (PVP-I), also known as iodopovidone, which is commonly used as an antiseptic for skin disinfection before and after surgery and works faster than either 0.04% PHMB on its own or hypochlorous acid (HOCI). Tests have shown that it can reduce planktonic bacteria levels by 99.99% in just one minute, and disrupted biofilm effectively.
Post-op problems
Taking into account the many complicating factors with the initial surgery, the procedure was at first highly successful and the wound was clinically unremarkable with good mobility of the patient and the range of motion was highly satisfactory. Consequently, the patient was discharged after one week. In the rehabilitation phase the patient experienced a sudden ‘cracking’ in the knee joint, followed by a short period of pain that soon subsided. Later, there was suture dehiscence – a separation of previously approximated wound edges due to a failure of proper wound healing – following the removal of the staples that had been used to close the wound. Furthermore, a 1.5cm fistula presented, as well as redness around the wound.
Poor healing is frequently observed in patients with diabetes mellitus, even if long-term glucose levels are wellmaintained, so the outcome of this operation was not entirely unforeseen. On returning to the clinic on day 21 after surgery, there was extensive redness on the wound area and the wound had become purulent. She was taken back to revision surgery.
“We did the debridement and implant retention procedure (DAIR) according to the guidelines to treat an early onset infection, and changed during revision surgery the mobile components of the knee (the polyethylene) to reduce potential biofilm wearing components,” explains Helwig. “For the DAIR procedure PREVENTIA was available and we used it for each revision surgery we performed on day 21 and on day 27. We did not know what germs would be inside the wound so we initially waited for five minutes to ensure that the broad antimicrobial effect of the irrigation had addressed any enterococci that might be present. If we leave PREVENTIA Surgical Irrigation in the joint for a short time there are additional effects that we might not get if we were using other substances,” he adds.
In the cultures there was a Staphylococcus aureus found in the wound and the periprothetic tissue. In addition to the surgery, she was administered Flucloxacillin IV for 14 days combined with Rifampicine after second revision surgery and healed wounds. With no wound inflammation signs and laboratory without any pathological findings, she was discharged from hospital with oral Cotrimoxazol and Rifampicin for an additional 6 weeks. The patient was seen monthly for three months in the outpatient clinic without any pathological findings, and she was very satisfied with the result.
“There are always different goals for patient outcomes,” says Helwig. “At first, it was pain reduction and mobility with a prosthesis, but when you have an infection, the infection-free implant becomes the goal. Then you want to ensure good function. We are happy the implant is still in place and that the infection has not recurred.”
Infection-free and with a new lease of life, thanks to PREVENTIA Surgical Irrigation and a skilled clinical team, meant that a very challenging case reached a successful conclusion.





